Decoding Urinary Frequency: Understanding ICD-10 Codes and What They Mean
Experiencing the constant urge to urinate can be disruptive and concerning. Understanding the potential causes and how healthcare professionals classify this symptom is crucial for effective diagnosis and treatment. This article delves into the world of urinary frequency, explaining what it is, the common causes, and the significance of ICD-10 codes in its diagnosis and management. We aim to provide a comprehensive resource that empowers you with knowledge and helps you navigate the complexities of this condition.
What is Urinary Frequency?
Urinary frequency refers to the need to urinate more often than usual. What’s considered ‘normal’ varies from person to person, but generally, most people urinate 4 to 8 times a day. If you find yourself needing to go significantly more often, especially if it’s interfering with your daily activities or sleep, it’s worth investigating. It’s important to distinguish urinary frequency from other urinary symptoms like urgency (a sudden, compelling need to urinate) and nocturia (frequent urination at night). While they can occur together, they each have distinct underlying causes.
ICD-10 Codes: A Universal Language for Diagnosis
ICD-10, or the International Classification of Diseases, 10th Revision, is a standardized coding system used by healthcare providers worldwide to classify and code diagnoses, symptoms, and procedures. These codes are essential for medical billing, data collection, and research. When you see a doctor for urinary frequency, they will use ICD-10 codes to document your condition. Understanding these codes can provide insight into the diagnostic process.
Specifically, when addressing urinary frequency, several ICD-10 codes might be relevant, depending on the underlying cause and any associated symptoms. The most common code directly related to urinary frequency is R35.0 – Frequency of micturition. However, this code often serves as a starting point, and further investigation is usually needed to determine the root cause. Other relevant codes might include those related to urinary tract infections (UTIs), overactive bladder (OAB), diabetes, or prostate issues in men. We will delve into these related conditions and their corresponding ICD-10 codes further below.
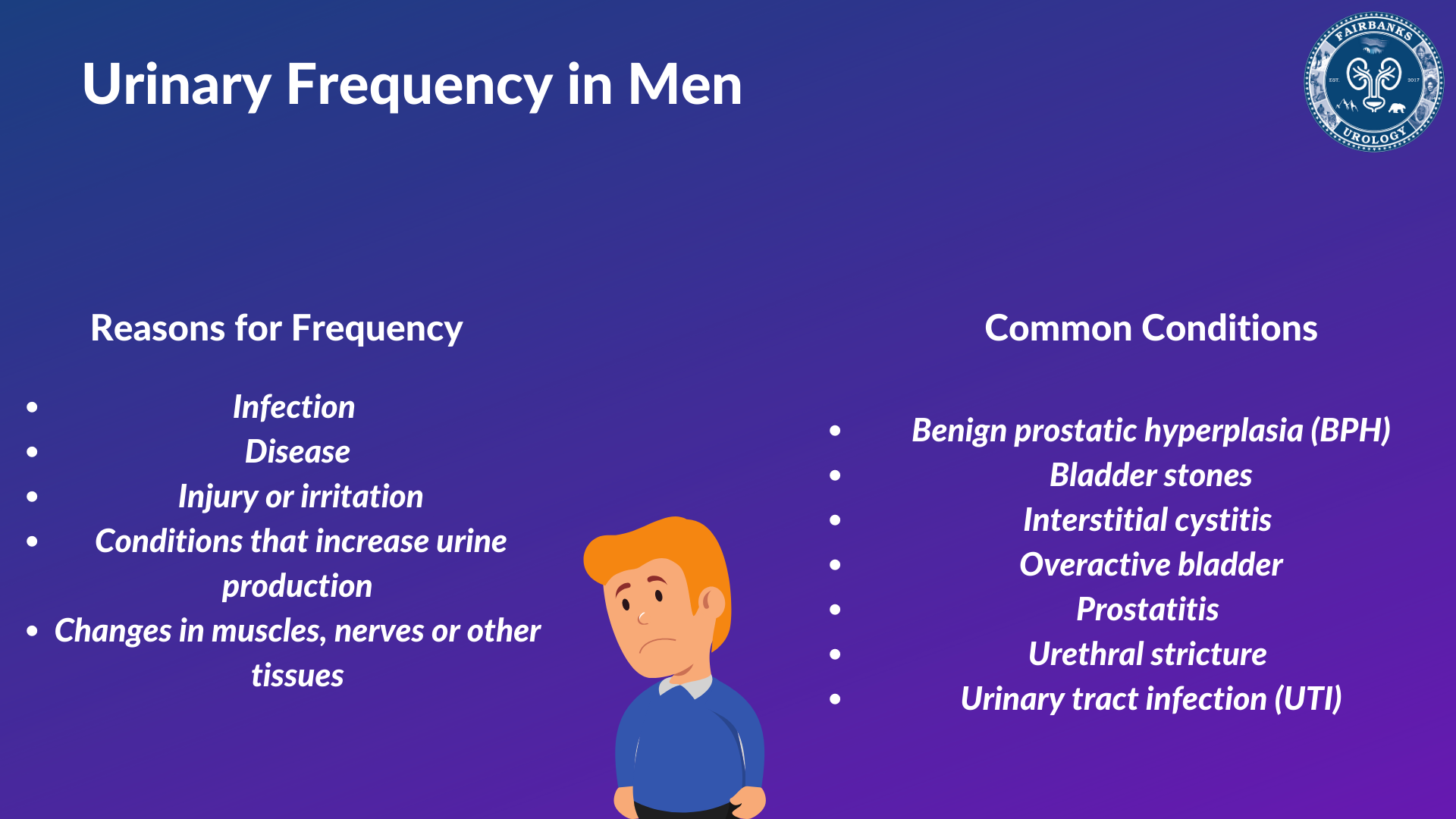
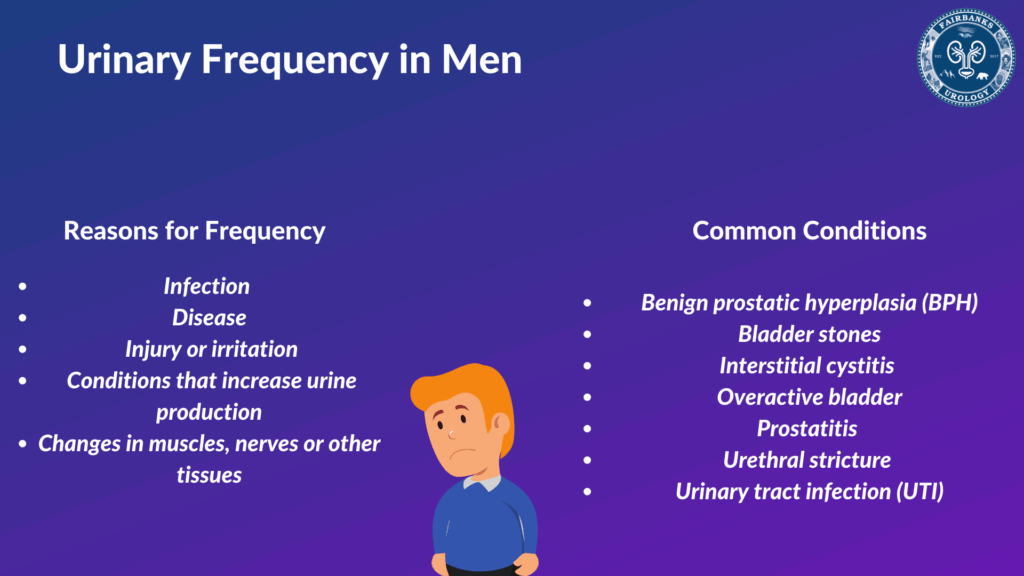
Common Causes of Urinary Frequency
Urinary frequency isn’t a disease itself, but rather a symptom of an underlying issue. Several factors can contribute to this increased need to urinate. Here are some of the most common causes:
- Urinary Tract Infections (UTIs): UTIs are a frequent culprit, especially in women. The infection irritates the bladder lining, leading to increased urgency and frequency. ICD-10 codes for UTIs vary depending on the location and specific bacteria involved (e.g., N39.0 for unspecified urinary tract infection).
- Overactive Bladder (OAB): OAB is a condition where the bladder muscles contract involuntarily, creating a sudden urge to urinate. This can lead to both urinary frequency and urgency. The ICD-10 code for overactive bladder is N32.81.
- Diabetes: High blood sugar levels in diabetes can lead to increased urine production as the body tries to eliminate excess glucose. Both type 1 and type 2 diabetes can cause urinary frequency. Relevant ICD-10 codes include E10-E14, depending on the type of diabetes and any associated complications.
- Prostate Issues (in men): An enlarged prostate (benign prostatic hyperplasia or BPH) can put pressure on the urethra, making it difficult to empty the bladder completely. This can lead to frequent urination, especially at night. The ICD-10 code for BPH is N40.
- Interstitial Cystitis (IC): Also known as painful bladder syndrome, IC is a chronic condition that causes bladder pain, pressure, and urinary frequency. The ICD-10 code for interstitial cystitis is N30.10.
- Diuretics: These medications, often prescribed for high blood pressure or fluid retention, increase urine production.
- Excessive Fluid Intake: Drinking large amounts of fluids, especially caffeinated beverages or alcohol, can naturally lead to more frequent urination.
- Pregnancy: The growing uterus puts pressure on the bladder, leading to increased frequency.
- Neurological Conditions: Conditions like multiple sclerosis (MS) or stroke can affect bladder control and lead to urinary frequency.
- Bladder Cancer: In rare cases, urinary frequency can be a symptom of bladder cancer.
Diagnosis and ICD-10 Codes: A Closer Look
Diagnosing the underlying cause of urinary frequency involves a thorough medical history, physical exam, and potentially some diagnostic tests. Your doctor will ask about your symptoms, fluid intake, medications, and any other relevant medical conditions. The physical exam may include a pelvic exam for women or a prostate exam for men. Diagnostic tests might include:
- Urinalysis: To check for infection, blood, or other abnormalities.
- Urine Culture: To identify any bacteria causing a UTI.
- Bladder Diary: To track your fluid intake and urination patterns.
- Post-Void Residual (PVR) Measurement: To measure the amount of urine left in your bladder after urination.
- Cystoscopy: To visualize the inside of the bladder and urethra.
- Urodynamic Testing: To assess bladder function and control.
The results of these tests, combined with your medical history and physical exam, will help your doctor determine the underlying cause of your urinary frequency and assign the appropriate ICD-10 code(s). Here’s how some common diagnoses relate to specific ICD-10 codes:
- UTI: As mentioned earlier, codes vary depending on the specific infection. For example, a UTI caused by E. coli might be coded as N39.0 (unspecified urinary tract infection) in conjunction with B96.20 (E. coli as the cause of diseases classified elsewhere).
- Overactive Bladder (OAB): N32.81. It’s important to note that this code can be further specified based on whether the OAB is wet (with urge incontinence) or dry (without urge incontinence).
- Diabetes: E10-E14. The specific code depends on the type of diabetes (type 1, type 2, etc.), whether it is controlled, and any associated complications (e.g., diabetic neuropathy affecting bladder function).
- Benign Prostatic Hyperplasia (BPH): N40. This code indicates an enlargement of the prostate gland.
- Interstitial Cystitis (IC): N30.10. This code specifically identifies non-ulcerative interstitial cystitis.
Treatment Options for Urinary Frequency
The treatment for urinary frequency depends entirely on the underlying cause. Once your doctor has identified the cause and assigned the appropriate ICD-10 code, they can develop a personalized treatment plan. Here are some common treatment options:
- Antibiotics for UTIs: Antibiotics are the standard treatment for bacterial UTIs. The specific antibiotic will depend on the bacteria identified in the urine culture.
- Medications for OAB: Several medications can help relax the bladder muscles and reduce the urge to urinate. These include antimuscarinics (e.g., oxybutynin, tolterodine) and beta-3 adrenergic agonists (e.g., mirabegron).
- Blood Sugar Control for Diabetes: Managing blood sugar levels through diet, exercise, and medication is crucial for reducing urinary frequency associated with diabetes.
- Medications or Surgery for BPH: Medications like alpha-blockers and 5-alpha reductase inhibitors can help relax the prostate muscles and shrink the prostate gland, respectively. In some cases, surgery may be necessary to remove part of the prostate.
- Pain Management and Bladder Training for IC: Treatment for IC focuses on managing pain and improving bladder control. This may involve medications, bladder training techniques, and lifestyle modifications.
- Lifestyle Modifications: Regardless of the underlying cause, certain lifestyle changes can help manage urinary frequency. These include limiting fluid intake before bed, avoiding caffeine and alcohol, and practicing bladder training techniques.
Beyond ICD-10: The Patient Experience
While ICD-10 codes provide a standardized way to classify and document medical conditions, it’s important to remember that they don’t capture the full patient experience. Living with urinary frequency can be frustrating, embarrassing, and disruptive. It can affect sleep, work, and social activities. That’s why it’s so important to seek medical help and work with your doctor to find a treatment plan that works for you. Don’t hesitate to openly communicate your symptoms and concerns, as this will help your doctor make an accurate diagnosis and develop the most effective treatment strategy. In our experience, patients who actively participate in their care and maintain open communication with their healthcare providers often experience the best outcomes.
The Role of Telehealth in Managing Urinary Frequency
In recent years, telehealth has emerged as a valuable tool for managing various health conditions, including urinary frequency. Telehealth offers several advantages, such as increased accessibility, convenience, and cost-effectiveness. Patients can consult with healthcare providers from the comfort of their own homes, eliminating the need for travel and reducing wait times. Telehealth can be particularly useful for initial consultations, follow-up appointments, and medication management. It also allows for remote monitoring of symptoms and adherence to treatment plans. As healthcare continues to evolve, telehealth is likely to play an increasingly important role in the management of urinary frequency and other urological conditions. Leading experts in urology suggest that telehealth can improve patient outcomes by facilitating timely access to care and promoting patient engagement.
Navigating Your Health: Understanding the Bigger Picture
Understanding urinary frequency and the associated ICD-10 codes is a crucial first step in managing this condition. However, it’s equally important to understand the broader context of your health. Consider factors such as your overall lifestyle, diet, exercise habits, and stress levels. These factors can significantly impact your bladder health and contribute to urinary frequency. Maintaining a healthy weight, eating a balanced diet, and engaging in regular physical activity can help improve bladder control and reduce urinary frequency. Stress management techniques, such as yoga, meditation, or deep breathing exercises, can also be beneficial. By taking a holistic approach to your health, you can empower yourself to manage urinary frequency and improve your overall well-being.
Taking Control of Your Bladder Health
Dealing with urinary frequency can be challenging, but understanding the potential causes and the role of ICD-10 codes is a significant step towards effective management. By working closely with your healthcare provider, you can identify the underlying cause of your symptoms and develop a personalized treatment plan that addresses your specific needs. Remember, you are not alone, and there are many resources available to help you regain control of your bladder health and improve your quality of life. If you’re experiencing frequent urination, don’t hesitate to seek medical advice. Early diagnosis and treatment can prevent complications and improve your overall well-being. Consider discussing your symptoms with your doctor and exploring the various treatment options available. The journey to better bladder health starts with a single step – taking control of your health and seeking the support you need.