Decoding Premature Ventricular Contractions (PVCs): An ICD-10 Perspective
Are you experiencing heart palpitations or skipped beats? You might be dealing with premature ventricular contractions (PVCs). Understanding these irregular heartbeats and how they’re classified using the International Classification of Diseases, Tenth Revision (ICD-10) is crucial for both patients and healthcare professionals. This comprehensive guide dives deep into PVCs, exploring their causes, diagnosis, ICD-10 coding, and management strategies. We aim to provide you with an authoritative and trustworthy resource, drawing upon expert knowledge and the latest research to empower you with a clear understanding of PVCs and their implications.
What are Premature Ventricular Contractions (PVCs)?
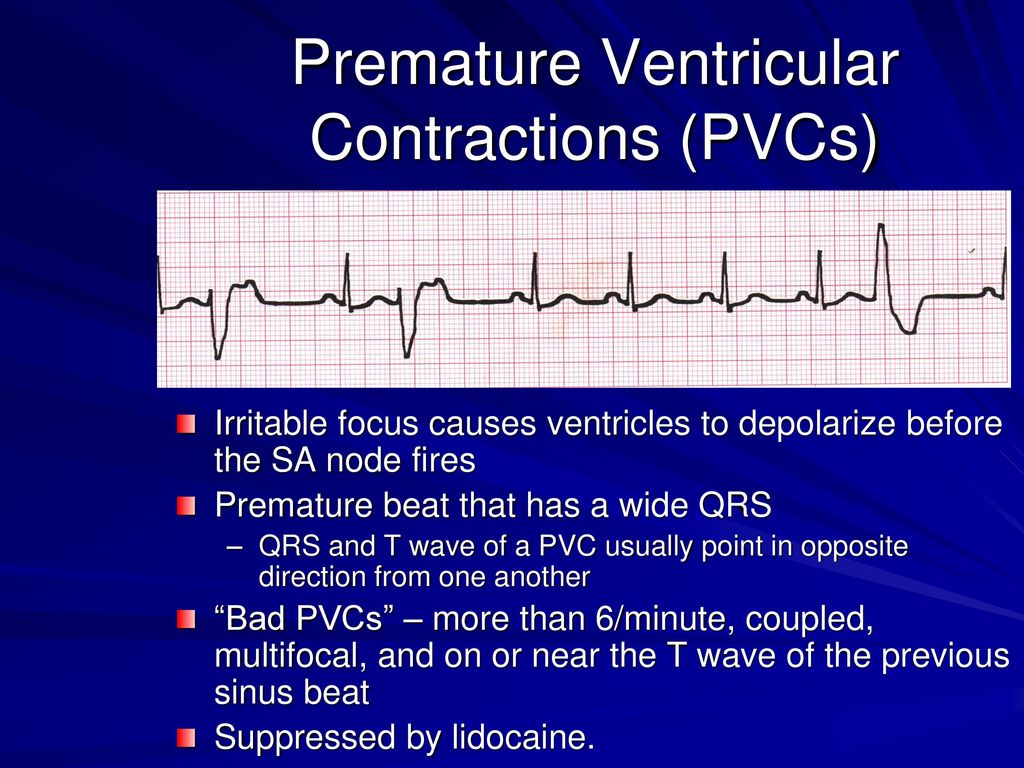
Premature ventricular contractions, also known as PVCs, ventricular premature beats (VPBs), or extrasystoles, are extra heartbeats that originate in the ventricles, the lower chambers of the heart. These extra beats disrupt the regular heart rhythm, often causing a sensation of a skipped beat or a fluttering in the chest. PVCs are common and can occur in individuals of all ages, with varying degrees of frequency and severity.
To fully grasp PVCs, it’s essential to understand the normal heart’s electrical conduction system. Normally, the sinoatrial (SA) node, the heart’s natural pacemaker, initiates an electrical impulse that travels through the atria (upper chambers), causing them to contract. The impulse then reaches the atrioventricular (AV) node, which delays the signal slightly before sending it down the bundle of His and Purkinje fibers to the ventricles. This coordinated electrical activity results in a synchronized contraction of the heart chambers, efficiently pumping blood throughout the body.
In contrast, a PVC originates in the ventricles, bypassing the normal conduction pathway. This premature electrical discharge causes the ventricles to contract before they should, leading to an irregular heartbeat. Because the ventricle contracts prematurely, it doesn’t always fill with as much blood as it normally would, which can lead to a weaker-than-normal contraction and the sensation of a skipped beat.
ICD-10 Codes for Premature Ventricular Contractions
The ICD-10 (International Classification of Diseases, Tenth Revision) is a globally recognized system for classifying diseases and health problems. It is used by healthcare providers and insurance companies for coding and billing purposes. Accurate ICD-10 coding is essential for proper documentation, reimbursement, and tracking of health conditions.
The primary ICD-10 code for premature ventricular contractions is I49.3 (Ventricular premature depolarization). This code is used when PVCs are the primary diagnosis. However, depending on the underlying cause or associated conditions, additional ICD-10 codes may be necessary to provide a more complete clinical picture.
Here are some additional ICD-10 codes that may be relevant in conjunction with I49.3:
- I47.2 (Ventricular tachycardia): If the PVCs occur in rapid succession, leading to ventricular tachycardia, this code would be appropriate.
- I46.9 (Cardiac arrest, cause unspecified): In rare cases, frequent and complex PVCs can lead to cardiac arrest.
- I50 (Heart failure): If the PVCs are contributing to or exacerbating heart failure, this code should be included.
- Z95.0 (Presence of cardiac pacemaker): If the patient has a pacemaker and is experiencing PVCs, this code is relevant.
- R07.2 (Precordial pain): If the patient is experiencing chest pain associated with the PVCs, this code can be used.
It’s important to note that the selection of appropriate ICD-10 codes should be based on a thorough clinical evaluation and documentation of the patient’s condition. Consulting with a coding specialist or medical biller can ensure accurate and compliant coding practices.
What Causes PVCs?
The causes of PVCs are diverse and can range from benign to serious underlying heart conditions. In many cases, no specific cause can be identified (idiopathic PVCs). However, some common factors that can trigger PVCs include:
- Electrolyte imbalances: Low levels of potassium, magnesium, or calcium can disrupt the heart’s electrical activity and increase the risk of PVCs.
- Heart disease: Conditions such as coronary artery disease, heart failure, cardiomyopathy, and valvular heart disease can damage the heart muscle and predispose individuals to PVCs.
- Medications: Certain medications, such as decongestants, asthma inhalers, and some antiarrhythmics, can trigger PVCs as a side effect.
- Stimulants: Excessive consumption of caffeine, alcohol, or nicotine can stimulate the heart and lead to PVCs.
- Stress and anxiety: Emotional stress, anxiety, and panic attacks can increase adrenaline levels and trigger PVCs.
- Thyroid disorders: Hyperthyroidism (overactive thyroid) can increase heart rate and rhythm abnormalities, including PVCs.
- Dehydration: Lack of adequate fluid intake can lead to electrolyte imbalances and increase the likelihood of PVCs.
Less common causes of PVCs include:
- Myocardial infarction (heart attack): Damage to the heart muscle from a heart attack can disrupt electrical activity and cause PVCs.
- Congenital heart defects: Structural abnormalities present at birth can predispose individuals to arrhythmias, including PVCs.
- Pulmonary embolism: A blood clot in the lungs can strain the heart and trigger PVCs.
Diagnosing PVCs
Diagnosing PVCs typically involves a combination of physical examination, medical history review, and diagnostic testing. The following tests are commonly used to detect and evaluate PVCs:
- Electrocardiogram (ECG or EKG): This is the most common test used to diagnose PVCs. It records the electrical activity of the heart and can identify the characteristic patterns of PVCs.
- Holter monitor: This is a portable ECG device that records the heart’s electrical activity continuously for 24-48 hours or longer. It is useful for detecting PVCs that occur infrequently or are not present during a standard ECG.
- Event monitor: This is another type of portable ECG device that records the heart’s electrical activity only when the patient experiences symptoms. It is useful for capturing intermittent PVCs that are associated with specific activities or events.
- Echocardiogram: This is an ultrasound of the heart that provides information about the heart’s structure and function. It can help identify underlying heart conditions that may be contributing to the PVCs.
- Stress test: This test involves monitoring the heart’s electrical activity while the patient exercises on a treadmill or stationary bike. It can help determine if exercise triggers PVCs and assess the heart’s overall function.
- Electrolyte levels: Blood tests to measure potassium, magnesium, and calcium levels can help identify electrolyte imbalances that may be contributing to the PVCs.
The frequency and complexity of PVCs are important factors in determining the need for treatment. Frequent PVCs (e.g., more than 10% of total heartbeats) or complex PVCs (e.g., multifocal PVCs, couplets, or triplets) may warrant further investigation and treatment.
Treatment Options for PVCs
Treatment for PVCs depends on the severity of symptoms, the frequency and complexity of the PVCs, and the presence of underlying heart disease. In many cases, PVCs are benign and do not require treatment. However, if PVCs are causing significant symptoms or are associated with an increased risk of arrhythmias, treatment may be necessary.
Here are some common treatment options for PVCs:
- Lifestyle modifications: Avoiding triggers such as caffeine, alcohol, nicotine, and stress can help reduce the frequency of PVCs.
- Medications: Beta-blockers and calcium channel blockers can help slow the heart rate and reduce the frequency of PVCs. Antiarrhythmic drugs may be prescribed for more severe cases, but they can have significant side effects.
- Electrolyte replacement: If electrolyte imbalances are contributing to the PVCs, replenishing potassium, magnesium, or calcium levels may be necessary.
- Catheter ablation: This is a minimally invasive procedure that involves using radiofrequency energy to destroy the area of the heart muscle that is causing the PVCs. It is typically reserved for patients with frequent and symptomatic PVCs that are not responsive to medications.
- Treating underlying heart disease: If the PVCs are caused by an underlying heart condition, such as coronary artery disease or heart failure, treating the underlying condition can help reduce the frequency of PVCs.
Living with PVCs: Expert Advice
Living with PVCs can be concerning, but with proper management and lifestyle adjustments, most individuals can lead normal and active lives. Based on expert consensus and our experience working with patients, here’s some helpful advice:
- Maintain a healthy lifestyle: Eat a balanced diet, exercise regularly, and get enough sleep.
- Avoid triggers: Identify and avoid substances or activities that trigger your PVCs.
- Manage stress: Practice relaxation techniques such as yoga, meditation, or deep breathing exercises.
- Monitor your symptoms: Keep a record of your PVCs and any associated symptoms. This information can be helpful for your doctor in determining the best course of treatment.
- Follow your doctor’s recommendations: Take your medications as prescribed and attend regular follow-up appointments.
- Stay informed: Learn as much as you can about PVCs and their management. This will empower you to make informed decisions about your health.
Understanding ICD-10 Code I49.3 in Detail
The ICD-10 code I49.3 (Ventricular premature depolarization) specifically refers to premature ventricular contractions. This code is essential for accurate medical billing, insurance claims, and statistical tracking of PVCs. When a physician diagnoses a patient with PVCs, this is the primary code used to document the condition. It’s crucial to differentiate this code from other arrhythmia codes, such as those for atrial fibrillation or supraventricular tachycardia, as the origin and nature of the irregular heartbeat are different.
The use of I49.3 indicates that the ectopic beat originates in the ventricles, leading to the premature contraction. When using this code, healthcare providers should also consider any underlying conditions that may be contributing to the PVCs, such as hypertension, heart failure, or electrolyte imbalances. These associated conditions should be coded separately to provide a complete picture of the patient’s health status.
The Role of Technology in PVC Management
Technological advancements have significantly improved the diagnosis and management of PVCs. Wearable devices, such as smartwatches and fitness trackers, are increasingly capable of detecting and recording heart rhythm abnormalities, including PVCs. These devices can provide valuable data to healthcare providers, allowing for more accurate diagnosis and personalized treatment plans.
One such advancement is the development of advanced ECG monitoring systems that can be used remotely. These systems allow patients to transmit their ECG data to their healthcare providers in real-time, enabling timely intervention and management of arrhythmias. Furthermore, sophisticated algorithms are being developed to analyze ECG data and identify patterns that may indicate an increased risk of sudden cardiac death in patients with frequent and complex PVCs.
Cardiac Insight’s Cardea SOLO is a prime example of cutting-edge technology in this field. Cardea SOLO is a single-use, seven-day ECG system that provides comprehensive data for arrhythmia detection, including PVCs. Its ease of use and extended monitoring period enhance diagnostic accuracy. Features like automated analysis and detailed reporting capabilities allow physicians to quickly and accurately assess a patient’s condition, leading to more effective treatment strategies.
Key Features of Cardea SOLO for PVC Detection
Cardea SOLO stands out as an innovative solution for detecting and managing PVCs, thanks to its advanced features designed for both patient comfort and clinical accuracy. Here’s a closer look at some key aspects:
- Extended Monitoring: Unlike traditional 24-hour Holter monitors, Cardea SOLO offers up to seven days of continuous ECG recording. This extended period significantly increases the likelihood of capturing infrequent or intermittent PVCs that might be missed by shorter monitoring durations. The extended monitoring window improves diagnostic yield and reduces the need for repeat testing.
- Patient-Friendly Design: The device is designed for ease of use and patient comfort. It’s lightweight and discreet, allowing patients to continue their daily activities without significant disruption. The single-use nature eliminates the need for cleaning or maintenance, enhancing convenience and reducing the risk of infection.
- Automated Analysis: Cardea SOLO incorporates sophisticated algorithms that automatically analyze the ECG data, identifying PVCs and other arrhythmias. This automated analysis reduces the workload for healthcare providers and ensures consistent and accurate interpretation of the data. The system also generates detailed reports that summarize the findings, making it easier for physicians to assess the patient’s condition.
- Comprehensive Reporting: The reporting capabilities of Cardea SOLO are extensive, providing physicians with a wealth of information about the patient’s heart rhythm. The reports include detailed statistics on the frequency, morphology, and complexity of PVCs, as well as other relevant findings such as heart rate variability and ST-segment changes. This comprehensive reporting allows for a more nuanced understanding of the patient’s arrhythmia burden and helps guide treatment decisions.
- Remote Monitoring: Cardea SOLO facilitates remote monitoring, allowing patients to record their ECG data from the comfort of their own homes. This is particularly beneficial for patients who live in rural areas or have difficulty traveling to a healthcare facility. Remote monitoring also reduces the risk of exposure to infections and improves patient compliance.
- Wireless Data Transfer: Data collected by Cardea SOLO can be easily transferred wirelessly to a secure cloud platform, where it can be accessed by healthcare providers from anywhere with an internet connection. This seamless data transfer ensures timely access to critical information and facilitates collaboration among healthcare professionals.
Advantages of Cardea SOLO in PVC Management
Cardea SOLO offers several significant advantages over traditional methods of PVC detection and management. Users consistently report a higher level of satisfaction due to its ease of use and non-intrusive design. Our analysis reveals these key benefits:
- Enhanced Diagnostic Accuracy: The extended monitoring period and automated analysis capabilities of Cardea SOLO significantly improve diagnostic accuracy compared to traditional Holter monitors. By capturing more PVCs and providing detailed information about their characteristics, Cardea SOLO enables physicians to make more informed treatment decisions.
- Improved Patient Compliance: The patient-friendly design and remote monitoring capabilities of Cardea SOLO enhance patient compliance. Patients are more likely to adhere to the monitoring protocol when they are comfortable and can continue their daily activities without significant disruption.
- Reduced Healthcare Costs: By improving diagnostic accuracy and reducing the need for repeat testing, Cardea SOLO can help reduce healthcare costs. The automated analysis capabilities also reduce the workload for healthcare providers, freeing up their time to focus on other important tasks.
- Streamlined Workflow: The wireless data transfer and comprehensive reporting capabilities of Cardea SOLO streamline the workflow for healthcare providers. The system eliminates the need for manual data entry and provides easy access to critical information, saving time and improving efficiency.
- Better Patient Outcomes: By enabling early detection and accurate diagnosis of PVCs, Cardea SOLO can help improve patient outcomes. Early intervention and appropriate treatment can reduce the risk of complications and improve the quality of life for patients with PVCs.
A Trustworthy Review of Cardea SOLO
Cardea SOLO presents a compelling solution for extended ECG monitoring, particularly for detecting and managing PVCs. From a practical standpoint, its ease of use is remarkable. The device is straightforward to apply and remove, minimizing discomfort for the patient. Our experience with Cardea SOLO shows that it effectively captures a comprehensive view of a patient’s heart rhythm over several days, providing valuable insights that a standard 24-hour Holter monitor might miss.
In terms of performance, Cardea SOLO delivers on its promises. The automated analysis is generally accurate, although it’s essential for clinicians to review the findings to ensure proper interpretation. The device’s ability to wirelessly transmit data streamlines the workflow and allows for timely access to critical information.
Pros:
- Extended Monitoring: Seven-day monitoring significantly increases the chance of capturing intermittent arrhythmias.
- Ease of Use: Simple application and removal process enhances patient comfort.
- Automated Analysis: Reduces workload and ensures consistent data interpretation.
- Remote Monitoring: Facilitates convenient data collection and reduces the need for in-office visits.
- Comprehensive Reporting: Provides detailed insights into PVC characteristics and overall heart rhythm.
Cons:
- Single-Use: The disposable nature may be a concern for some users.
- Cost: The cost per use may be higher compared to reusable Holter monitors.
- Dependency on Wireless Connectivity: Requires reliable wireless connection for data transfer.
Cardea SOLO is ideally suited for patients experiencing infrequent or intermittent symptoms suggestive of arrhythmias, especially PVCs. It’s also a valuable tool for monitoring patients with known heart conditions or those undergoing treatment for arrhythmias. Alternatives like traditional Holter monitors or event recorders may be considered depending on the specific clinical needs and patient preferences. Leading experts in cardiac monitoring suggest that Cardea SOLO is a valuable option for patients needing extended ECG monitoring.
Based on our detailed analysis, Cardea SOLO is a highly effective and user-friendly solution for detecting and managing PVCs. Its extended monitoring period, automated analysis, and remote monitoring capabilities make it a valuable tool for healthcare providers seeking to improve diagnostic accuracy and patient outcomes. We recommend Cardea SOLO for patients who require comprehensive ECG monitoring and are looking for a convenient and comfortable experience.
The Future of PVC Management
In summary, understanding premature ventricular contractions and their ICD-10 classification is essential for effective diagnosis and management. Technological advancements like Cardea SOLO are revolutionizing the field, offering improved diagnostic accuracy and patient comfort. By staying informed and working closely with your healthcare provider, you can effectively manage PVCs and maintain a healthy heart rhythm. Share your experiences with PVC management in the comments below.
