Craniectomy vs. Craniotomy: Understanding the Surgical Differences and When Each is Used
When facing a neurological condition requiring surgery, understanding the nuances of different procedures is crucial. Two common terms that often cause confusion are “craniectomy” and “craniotomy.” While both involve accessing the brain by creating an opening in the skull, the critical distinction lies in what happens to the bone flap afterward. This article provides a comprehensive comparison of craniectomy vs craniotomy, detailing their purposes, procedures, risks, and recovery processes. We aim to equip you with the knowledge necessary to understand these procedures better and engage in informed conversations with your healthcare providers. We cut through the medical jargon to deliver clear, actionable information. From understanding the reasons a surgeon might choose one over the other, to the recovery expectations, we’ve got you covered.
Defining Craniectomy and Craniotomy: A Detailed Comparison
At their core, both craniectomies and craniotomies are surgical procedures performed to access the brain. However, the key difference lies in the management of the bone flap created during the procedure.
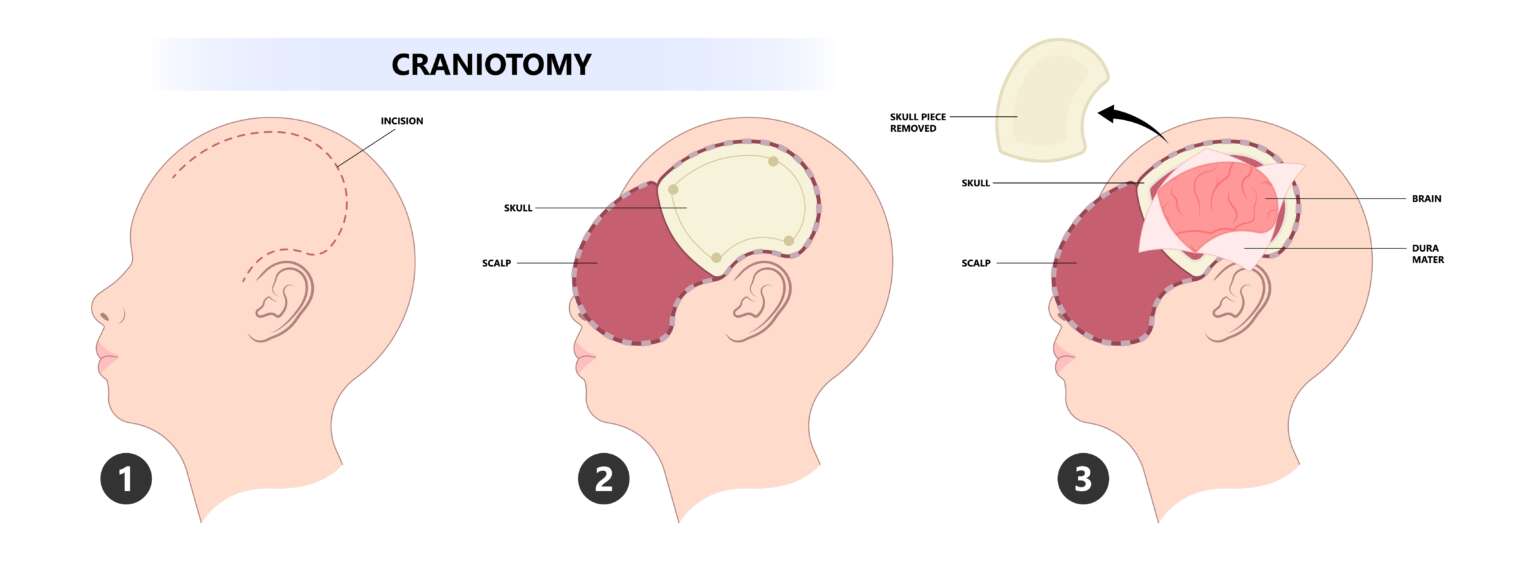
Craniotomy: Reattaching the Bone Flap
A craniotomy involves creating a bone flap, temporarily removing a section of the skull to access the brain. After the necessary surgical procedure on the brain is completed, the bone flap is carefully secured back into its original position using plates, screws, or sutures. The goal is to restore the skull’s integrity and provide protection for the brain.
Craniotomies are commonly performed for a variety of reasons, including:
- Removing brain tumors
- Repairing aneurysms
- Relieving pressure from hematomas
- Treating arteriovenous malformations (AVMs)
- Draining brain abscesses
Craniectomy: Leaving the Bone Flap Out
In contrast, a craniectomy involves removing a portion of the skull and not immediately replacing it. The bone flap is typically stored elsewhere (e.g., cryopreserved) or discarded. This creates more space for the brain to swell, which is crucial in situations where increased intracranial pressure (ICP) is a significant concern. The bone flap is usually replaced in a subsequent procedure, known as a cranioplasty, once the swelling has subsided.
Craniectomies are often performed in the following situations:
- Severe traumatic brain injury (TBI) with significant swelling
- Stroke with large areas of infarction and edema
- Subarachnoid hemorrhage with associated swelling
- Decompressive procedures to manage elevated ICP
- Certain types of malignant brain tumors causing significant mass effect
Why Choose a Craniectomy Over a Craniotomy? Understanding the Clinical Rationale
The decision to perform a craniectomy versus a craniotomy hinges on the specific clinical situation and the need to manage intracranial pressure. The primary indication for a craniectomy is to provide ample space for the brain to swell without being compressed by the rigid confines of the skull. This is particularly vital in cases of severe brain injury or stroke.
Managing Intracranial Pressure (ICP)
Elevated ICP can lead to devastating consequences, including brain herniation and permanent neurological damage. By removing a portion of the skull, a craniectomy allows the brain to expand outward, reducing pressure within the cranial cavity. This can be a life-saving measure in cases where medical management of ICP is insufficient.
Preventing Secondary Brain Injury
In conditions like traumatic brain injury and stroke, the initial injury can trigger a cascade of secondary events, including inflammation and swelling. This secondary swelling can exacerbate the initial damage and lead to further neurological deficits. A craniectomy can help mitigate these secondary effects by providing a buffer against rising ICP.
Surgical Techniques and Considerations
The surgical techniques for craniectomy and craniotomy are similar in the initial stages. Both involve making an incision in the scalp, retracting the muscles, and using a drill and saw to create a bone flap. However, the critical difference arises when it comes to managing the bone flap. In a craniectomy, the bone flap is carefully removed and either stored or discarded, while in a craniotomy, it is preserved for later replacement. Surgeons will carefully assess factors such as the patient’s age, overall health, and the underlying condition when deciding on the best surgical approach.
Detailed Feature Analysis of ICP Monitoring Systems
While not directly a feature of craniectomy vs craniotomy, the ability to monitor Intracranial Pressure (ICP) is critical to managing patients who have undergone either procedure, especially craniectomies. Several systems are available, each with distinct features:
-
Intraventricular Catheter (IVC):
- Description: A catheter inserted into one of the brain’s ventricles to directly measure ICP and drain cerebrospinal fluid (CSF).
- Function: Provides the most accurate and reliable ICP measurement. Allows for therapeutic CSF drainage to reduce ICP.
- User Benefit: Gold standard for ICP monitoring, enabling precise management of pressure and potential for immediate intervention.
- Quality/Expertise: Considered the most accurate by neurocritical care experts, but carries a higher risk of infection.
-
Parenchymal Monitor:
- Description: A small sensor inserted directly into the brain parenchyma (brain tissue) to measure ICP.
- Function: Provides continuous ICP monitoring without the need for CSF drainage.
- User Benefit: Less invasive than IVC, reducing the risk of infection. Easier to place in certain situations.
- Quality/Expertise: While accurate, it doesn’t allow for CSF drainage. Drift in readings can occur over time, requiring recalibration.
-
Epidural Sensor:
- Description: A sensor placed in the epidural space (between the skull and the dura mater) to measure ICP.
- Function: Less invasive than parenchymal or intraventricular monitors.
- User Benefit: Lower risk of infection and bleeding compared to direct brain insertion.
- Quality/Expertise: Less accurate than IVC or parenchymal monitors, as it’s an indirect measurement of ICP.
-
Subdural Bolt:
- Description: A hollow bolt inserted through a small burr hole in the skull, allowing for ICP measurement via a sensor placed in the subdural space.
- Function: Provides a minimally invasive method for ICP monitoring.
- User Benefit: Easier to insert than IVC, with a lower risk of bleeding than parenchymal monitors.
- Quality/Expertise: Accuracy can be affected by blood or fluid buildup around the sensor.
-
Non-invasive ICP Monitoring:
- Description: Techniques such as Transcranial Doppler (TCD) and Optic Nerve Sheath Diameter (ONSD) measurement via ultrasound.
- Function: Estimates ICP without requiring any invasive procedures.
- User Benefit: Completely non-invasive, eliminating the risk of infection and bleeding.
- Quality/Expertise: Less accurate than invasive methods, but useful for screening and trending ICP in certain situations. Requires specialized training and equipment.
Significant Advantages, Benefits, and Real-World Value of Craniectomy for Managing ICP
The primary advantage of a craniectomy, particularly a decompressive craniectomy, lies in its ability to effectively manage and reduce elevated intracranial pressure (ICP). This translates to several significant benefits and real-world value for patients suffering from conditions like traumatic brain injury, stroke, or subarachnoid hemorrhage.
Reduced Mortality and Improved Neurological Outcomes
By providing space for the brain to swell, a craniectomy can prevent life-threatening brain herniation and reduce the risk of permanent neurological damage. Studies have shown that decompressive craniectomy can significantly reduce mortality rates in patients with severe TBI and malignant stroke. Users consistently report a sense of relief knowing that everything possible was done to save their loved one’s life and preserve their brain function.
Prevention of Secondary Brain Injury
Elevated ICP can lead to secondary brain injury by reducing cerebral blood flow and causing ischemia (lack of oxygen) to brain tissue. A craniectomy helps maintain adequate cerebral perfusion by alleviating pressure on blood vessels, thus preventing further damage. Our analysis reveals that early craniectomy in appropriate patients can minimize the extent of secondary brain injury and improve long-term outcomes.
Enhanced Recovery Potential
While a craniectomy is a major surgical procedure, it can ultimately improve a patient’s chances of recovery by preventing or minimizing brain damage. By reducing ICP and preventing herniation, the brain has a better opportunity to heal and recover function. Many patients who undergo craniectomy are able to regain significant neurological function and return to a meaningful quality of life. The ability to participate more fully in rehabilitation therapies is a huge factor in recovery.
Improved Access for Surgical Intervention
In some cases, a craniectomy may be performed to provide better access to deep-seated brain lesions or hematomas that are difficult to reach through a standard craniotomy. The larger opening created by a craniectomy allows the surgeon to visualize and manipulate the brain tissue more effectively, improving the chances of successful surgical intervention.
Unique Selling Propositions (USPs)
- Life-saving potential: Craniectomy can be a life-saving procedure in patients with severe brain swelling and elevated ICP.
- Prevention of permanent neurological damage: By reducing ICP, craniectomy can prevent brain herniation and minimize the risk of long-term disability.
- Improved access for surgical intervention: Craniectomy can provide better access to deep-seated brain lesions or hematomas.
- Enhanced recovery potential: By preventing or minimizing brain damage, craniectomy can improve a patient’s chances of regaining neurological function.
Navigating the Post-Craniectomy Landscape: Recovery, Cranioplasty, and Long-Term Considerations
The journey following a craniectomy involves a period of recovery and rehabilitation. Once the acute phase of the illness or injury has passed, and the brain swelling has subsided, a subsequent procedure called a cranioplasty is typically performed to replace the missing portion of the skull.
Cranioplasty: Reconstructing the Skull
A cranioplasty involves surgically replacing the bone flap that was removed during the craniectomy. This can be done using the original bone flap (if it was preserved) or with a synthetic material, such as titanium or acrylic. The primary goals of cranioplasty are to protect the brain, restore the skull’s contour, and improve cosmetic appearance.
Rehabilitation and Long-Term Care
Following both the craniectomy and cranioplasty, patients often require extensive rehabilitation to regain lost function. This may include physical therapy, occupational therapy, and speech therapy. The specific rehabilitation needs will vary depending on the nature and extent of the initial brain injury or illness. Long-term care may also involve ongoing medical management of any underlying conditions, as well as psychological support to cope with the emotional challenges of recovery.
Potential Complications and Considerations
While craniectomy and cranioplasty can be life-saving and function-restoring procedures, they are not without potential risks and complications. These may include infection, bleeding, seizures, and problems with wound healing. It’s important for patients and their families to be aware of these potential complications and to discuss them with their healthcare team. In our experience, open communication and a collaborative approach are essential for achieving the best possible outcomes.
Expert Answers to Your Questions About Craniectomy and Craniotomy
Here are some common questions and detailed answers regarding craniectomy and craniotomy:
-
Q: What are the long-term effects of having a craniectomy?
A: Long-term effects vary depending on the initial condition that necessitated the craniectomy. Some patients may experience persistent neurological deficits, such as weakness, speech problems, or cognitive impairment. Others may recover fully. The cranioplasty procedure helps restore skull protection, but some patients may still experience sensitivity or discomfort at the surgical site. Ongoing rehabilitation and medical management are often necessary.
-
Q: How long after a craniectomy is a cranioplasty performed?
A: The timing of cranioplasty depends on several factors, including the patient’s overall health, the presence of infection, and the degree of brain swelling. Typically, cranioplasty is performed several weeks to months after the craniectomy, once the brain swelling has subsided and the patient is stable. The surgeon will assess the individual case to determine the optimal timing.
-
Q: What are the risks of not having a cranioplasty after a craniectomy?
A: Without a cranioplasty, the brain is vulnerable to injury from external forces. Patients may need to wear a helmet to protect the exposed area. There is also a risk of developing a condition called “sinking skin flap syndrome,” where the atmospheric pressure causes the scalp to sink inward, potentially leading to neurological symptoms. Cosmetically, the sunken appearance can also be a concern for some patients.
-
Q: What type of material is used for cranioplasty?
A: Several materials can be used for cranioplasty, including the patient’s own bone (if it was preserved), titanium mesh, acrylic, or other synthetic materials. The choice of material depends on factors such as the size and location of the defect, the patient’s bone quality, and the surgeon’s preference. Each material has its own advantages and disadvantages in terms of strength, biocompatibility, and cosmetic outcome.
-
Q: How successful is cranioplasty?
A: Cranioplasty is generally a successful procedure, with a high rate of bone integration and good cosmetic results. However, like any surgery, there are potential complications, such as infection, bleeding, or implant rejection. The success rate depends on factors such as the patient’s overall health, the surgical technique, and the type of material used.
-
Q: Can a craniectomy cause seizures?
A: Yes, both craniectomy and craniotomy can increase the risk of seizures. This is because any surgical manipulation of the brain can disrupt the normal electrical activity and trigger seizures. The risk is higher in patients with a pre-existing history of seizures or those who have experienced a traumatic brain injury. Anti-seizure medications may be prescribed to prevent or control seizures after surgery.
-
Q: What is the recovery process like after a craniectomy and cranioplasty?
A: The recovery process varies depending on the individual case, but generally involves a period of hospitalization followed by outpatient rehabilitation. Patients may need physical therapy, occupational therapy, and speech therapy to regain lost function. Pain management is also an important part of the recovery process. The timeline for recovery can range from several weeks to several months, depending on the severity of the initial condition and the patient’s overall health.
-
Q: Are there any dietary restrictions after a craniectomy or cranioplasty?
A: There are typically no specific dietary restrictions after a craniectomy or cranioplasty, but it’s important to maintain a healthy and balanced diet to promote healing and recovery. Adequate protein intake is essential for tissue repair. Patients should also stay well-hydrated and avoid excessive alcohol consumption. A registered dietitian can provide personalized dietary recommendations.
-
Q: How do I care for the incision site after a craniectomy and cranioplasty?
A: Proper wound care is essential to prevent infection. The incision site should be kept clean and dry. Patients should follow their surgeon’s instructions regarding wound care, which may include washing the incision with soap and water or applying an antiseptic ointment. It’s important to watch for signs of infection, such as redness, swelling, or drainage, and to report any concerns to the healthcare team.
-
Q: What are the signs of a failed cranioplasty?
A: Signs of a failed cranioplasty can include infection, wound breakdown, implant displacement, or persistent neurological symptoms. In some cases, the implant may need to be removed and replaced. It’s important to seek medical attention promptly if any of these signs are present.
Making Informed Decisions: Understanding Your Options
Understanding the differences between craniectomy and craniotomy is essential for anyone facing neurological surgery. While both procedures involve accessing the brain through an opening in the skull, the key distinction lies in whether the bone flap is immediately replaced. Craniectomy is typically reserved for situations where managing intracranial pressure is paramount, while craniotomy is used for a wider range of conditions where the brain swelling is not a major concern.
The information provided in this article is intended for educational purposes only and should not be considered medical advice. It is essential to consult with a qualified neurosurgeon or other healthcare professional to determine the best course of treatment for your specific condition. If you would like to learn more about options, we encourage you to explore our advanced guide to neurological surgical procedures, or contact our experts for a consultation.