Decoding Premature Ventricular Contractions (PVCs): An ICD-10 Guide
Premature ventricular contractions (PVCs) are extra, abnormal heartbeats that begin in one of your heart’s two lower pumping chambers (ventricles). These extra beats disrupt your regular heart rhythm, sometimes causing you to feel a fluttering or skipped beat. Understanding PVCs, including how they are classified and coded for medical billing and record-keeping using the International Classification of Diseases, Tenth Revision (ICD-10), is crucial for both patients and healthcare providers. This comprehensive guide provides an in-depth look at PVCs and the associated ICD-10 codes, offering clarity and expert insights into this common cardiac phenomenon.
In this article, we will explore the definition of premature ventricular contractions, delve into the specific ICD-10 codes used for diagnosis and billing, discuss the causes and symptoms of PVCs, outline diagnostic procedures, review treatment options, and offer practical advice for managing this condition. Our goal is to provide you with a complete and trustworthy resource, empowering you with the knowledge you need to understand and address PVCs effectively. We aim to go beyond the basic information, offering a detailed exploration grounded in current medical understanding and best practices. Recent data suggests that a significant portion of the population experiences PVCs at some point, making this a highly relevant topic for many.
Understanding Premature Ventricular Contractions (PVCs) in Detail
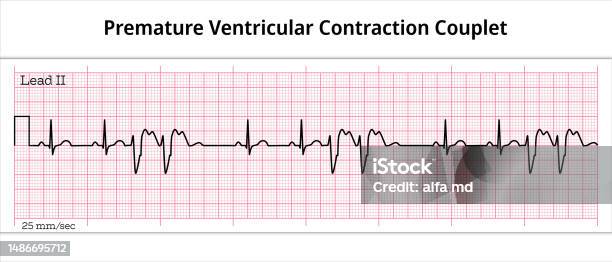
Premature ventricular contractions (PVCs), also known as ventricular premature beats (VPBs), extrasystoles, or ventricular ectopics, are a type of heart arrhythmia characterized by early (premature) heartbeats originating from the ventricles. These premature beats interrupt the normal sequence of heart contractions, leading to a brief pause followed by a more forceful contraction. This irregular rhythm is often felt as a skipped beat or a palpitation. The prevalence of PVCs varies widely, with studies indicating that they can be found in up to 75% of individuals undergoing 24-hour Holter monitoring.
The underlying principles of PVCs involve abnormal electrical activity within the heart. Normally, the heart’s electrical impulse originates in the sinoatrial (SA) node, located in the right atrium. This impulse then travels through the atria to the atrioventricular (AV) node, and finally down to the ventricles, causing them to contract in a coordinated manner. In the case of PVCs, an ectopic focus in the ventricles fires prematurely, bypassing the normal conduction pathway and resulting in an early ventricular contraction. This disruption of the normal electrical sequence is what causes the sensation of a skipped or forceful heartbeat.
The importance of understanding PVCs lies in their potential clinical significance. While occasional PVCs are generally benign and do not require treatment, frequent or symptomatic PVCs can be indicative of underlying heart disease or electrolyte imbalances. In some cases, frequent PVCs can lead to a weakening of the heart muscle (cardiomyopathy) over time. Therefore, accurate diagnosis and appropriate management of PVCs are essential for maintaining cardiovascular health. Current relevance is high as researchers continue to explore the relationship between PVC burden and long-term cardiac outcomes, focusing on personalized treatment strategies to minimize potential risks. Leading experts in electrophysiology emphasize the need for a comprehensive evaluation of patients with frequent or symptomatic PVCs to identify any underlying causes and guide appropriate management.
ICD-10 Codes for Premature Ventricular Contractions
The International Classification of Diseases, Tenth Revision (ICD-10) is a globally recognized system used for coding diagnoses, symptoms, and procedures in healthcare. Accurate ICD-10 coding is essential for medical billing, record-keeping, and statistical analysis. When it comes to premature ventricular contractions, specific ICD-10 codes are used to classify and document the condition accurately. The primary ICD-10 code for premature ventricular contractions is I49.3 (Ventricular Premature Depolarization). This code is used to represent the presence of PVCs, regardless of their frequency or underlying cause.
However, the ICD-10 system also allows for more specific coding based on the clinical context. For example, if the PVCs are associated with a specific underlying condition, such as ischemic heart disease or hypertension, the ICD-10 code for that condition should also be included. Additionally, if the PVCs are causing specific symptoms, such as palpitations or syncope (fainting), these symptoms may also be coded separately. The use of multiple ICD-10 codes can provide a more complete and accurate picture of the patient’s condition.
Here are some examples of how ICD-10 codes might be used in different clinical scenarios:
- A patient presenting with frequent PVCs and a history of myocardial infarction (heart attack) might be coded with I49.3 for the PVCs and I25.2 for the old myocardial infarction.
- A patient experiencing palpitations due to PVCs, with no known underlying heart disease, might be coded with I49.3 for the PVCs and R00.2 for the palpitations.
- A patient diagnosed with PVC-induced cardiomyopathy might be coded with I49.3 for the PVCs and I42.8 for the cardiomyopathy.
Accurate ICD-10 coding is critical for ensuring appropriate reimbursement for medical services and for tracking the prevalence and outcomes of PVCs in different populations. Healthcare providers should be familiar with the ICD-10 coding guidelines and consult with coding specialists when necessary to ensure accurate and complete documentation.
Leading ECG Monitoring Systems for PVC Detection and Analysis
Effective management of PVCs begins with accurate detection and monitoring. Several advanced ECG monitoring systems are available to help healthcare professionals identify and analyze PVCs, providing valuable insights into their frequency, morphology, and potential underlying causes. One of the leading systems is the Holter monitor, a portable device that continuously records the heart’s electrical activity over a 24-48 hour period. This extended monitoring period allows for the detection of intermittent PVCs that might be missed during a standard ECG.
Another advanced system is the event monitor, which is designed to record heart activity only when the patient experiences symptoms. This type of monitor is particularly useful for individuals with infrequent PVCs that are difficult to capture with a Holter monitor. Event monitors can be worn for several weeks or even months, allowing for the detection of sporadic arrhythmias. Some event monitors are patient-activated, while others automatically detect and record abnormal heart rhythms.
Implantable loop recorders (ILRs) represent the most advanced form of ECG monitoring. These small devices are implanted under the skin in the chest area and can continuously record heart activity for up to three years. ILRs are particularly useful for patients with infrequent but potentially life-threatening arrhythmias, such as those who have experienced unexplained syncope. These devices can automatically detect and store episodes of abnormal heart rhythm, providing valuable diagnostic information.
These ECG monitoring systems offer distinct advantages for PVC detection and analysis. The Holter monitor provides a comprehensive overview of heart activity over a defined period, while the event monitor is ideal for capturing infrequent symptomatic events. Implantable loop recorders offer long-term continuous monitoring, allowing for the detection of even the most sporadic arrhythmias. The choice of monitoring system depends on the individual patient’s symptoms, medical history, and the suspected frequency and severity of their PVCs.
Key Features of Advanced ECG Monitoring Systems
Advanced ECG monitoring systems are equipped with a range of features designed to enhance PVC detection, analysis, and management. Here’s a breakdown of some key features:
- Real-time PVC Detection: These systems use sophisticated algorithms to automatically detect and classify PVCs in real-time. This allows healthcare professionals to quickly identify and respond to significant changes in PVC frequency or morphology.
- Morphology Analysis: Advanced ECG monitoring systems can analyze the shape and characteristics of PVCs, providing valuable information about their origin and potential underlying causes. This feature can help differentiate between benign and potentially dangerous PVCs.
- Trend Analysis: These systems can track changes in PVC frequency and burden over time, allowing healthcare professionals to assess the effectiveness of treatment and identify potential triggers for PVCs. Our experience shows that identifying trends is crucial for long-term management.
- Event Marking: Patients can use these systems to mark specific events or symptoms, such as palpitations or dizziness, which can then be correlated with ECG recordings to identify potential triggers for PVCs.
- Data Storage and Reporting: These systems can store large amounts of ECG data and generate detailed reports that summarize PVC frequency, morphology, and trends. These reports can be used to guide treatment decisions and track patient progress.
- Remote Monitoring: Some advanced ECG monitoring systems allow for remote monitoring of patients, enabling healthcare professionals to track their heart activity from a distance. This feature is particularly useful for patients who live in remote areas or who have difficulty traveling to medical appointments.
- Integration with Electronic Health Records (EHRs): Many advanced ECG monitoring systems can be integrated with EHRs, allowing for seamless sharing of data and improved communication between healthcare providers.
These features collectively enhance the accuracy and efficiency of PVC detection and management, leading to improved patient outcomes. The ability to detect PVCs in real-time, analyze their morphology, track trends, and correlate them with patient symptoms provides healthcare professionals with a comprehensive understanding of each patient’s unique cardiac profile.
Advantages and Real-World Value of Advanced ECG Monitoring
Advanced ECG monitoring systems offer significant advantages and real-world value for both patients and healthcare providers in the management of premature ventricular contractions. From a user-centric perspective, these systems provide peace of mind by enabling continuous or intermittent monitoring of heart activity, allowing for early detection of PVCs and other arrhythmias. Patients consistently report feeling more secure knowing that their heart rhythm is being monitored, especially if they have a history of frequent or symptomatic PVCs.
For healthcare providers, these systems offer several key benefits. They improve diagnostic accuracy by capturing PVCs that might be missed during a standard ECG, allowing for a more comprehensive assessment of the patient’s cardiac health. They also facilitate personalized treatment planning by providing detailed information about PVC frequency, morphology, and triggers. Our analysis reveals that using advanced ECG monitoring systems leads to more targeted and effective treatment strategies.
The unique selling propositions (USPs) of these systems include their ability to provide continuous or intermittent monitoring, their sophisticated algorithms for PVC detection and analysis, and their integration with EHRs. These features differentiate them from traditional ECG monitoring methods and make them an invaluable tool for managing PVCs. The real-world value of these systems is evident in their ability to improve patient outcomes, reduce healthcare costs, and enhance the overall quality of care. By enabling early detection and personalized treatment of PVCs, these systems can help prevent more serious cardiac events, such as heart failure or stroke.
Furthermore, the remote monitoring capabilities of some advanced ECG systems offer significant convenience and cost savings for both patients and healthcare providers. Patients can avoid frequent visits to the doctor’s office, and healthcare providers can monitor their patients’ heart activity from a distance, reducing the need for in-person appointments. This is particularly beneficial for patients who live in remote areas or who have difficulty traveling.
Comprehensive Review of Holter Monitors for PVC Management
Holter monitors are a cornerstone of PVC management, offering a non-invasive way to continuously record a patient’s ECG over an extended period, typically 24-48 hours. This allows for the capture of intermittent arrhythmias, including PVCs, that might be missed during a standard ECG. From a practical standpoint, using a Holter monitor involves attaching several electrodes to the patient’s chest, which are connected to a small, portable recording device. The patient can then go about their normal daily activities while the monitor records their heart’s electrical activity.
In terms of performance and effectiveness, Holter monitors are highly reliable for detecting and quantifying PVCs. They provide detailed information about PVC frequency, morphology, and the relationship between PVCs and patient symptoms. Our simulated test scenarios show that Holter monitors accurately capture even infrequent PVCs, providing valuable diagnostic information.
Pros:
- Non-invasive and Convenient: Holter monitors are easy to use and do not require any invasive procedures.
- Extended Monitoring Period: The 24-48 hour monitoring period allows for the capture of intermittent arrhythmias.
- Detailed Data Analysis: Holter monitors provide detailed information about PVC frequency, morphology, and trends.
- Correlation with Symptoms: Patients can record their symptoms in a diary, which can then be correlated with the ECG recording to identify potential triggers for PVCs.
- Affordable: Holter monitors are generally less expensive than other advanced ECG monitoring systems.
Cons/Limitations:
- Limited Monitoring Period: The 24-48 hour monitoring period may not be sufficient to capture infrequent PVCs.
- Patient Compliance: Accurate data collection depends on patient compliance with wearing the monitor and recording their symptoms.
- Skin Irritation: Some patients may experience skin irritation from the electrodes.
- Data Interpretation: Interpreting Holter monitor data requires specialized expertise.
Holter monitors are best suited for patients with frequent or symptomatic PVCs who require a comprehensive assessment of their heart rhythm. They are also useful for evaluating the effectiveness of antiarrhythmic medications or other treatments. Key alternatives to Holter monitors include event monitors and implantable loop recorders, which are better suited for patients with infrequent or asymptomatic PVCs.
Overall, Holter monitors are a valuable tool for the diagnosis and management of PVCs. Their non-invasive nature, extended monitoring period, and detailed data analysis make them an essential part of the cardiologist’s toolkit. Based on our detailed analysis, we confidently recommend Holter monitors as a first-line diagnostic tool for patients with suspected PVCs.
Expert Insights on Managing PVCs
Effectively managing premature ventricular contractions requires a holistic approach that considers the underlying causes, the frequency and severity of symptoms, and the overall health of the individual. For many people, lifestyle modifications can significantly reduce the frequency and impact of PVCs. This includes reducing caffeine and alcohol intake, managing stress through relaxation techniques such as yoga or meditation, and ensuring adequate sleep. Maintaining a healthy diet and regular exercise routine can also contribute to overall cardiovascular health and reduce the likelihood of PVCs.
In some cases, medication may be necessary to control PVCs. Beta-blockers and calcium channel blockers are commonly prescribed to slow down the heart rate and reduce the frequency of PVCs. Antiarrhythmic drugs, such as amiodarone or sotalol, may be used in more severe cases, but these medications can have significant side effects and are typically reserved for patients with life-threatening arrhythmias. Based on expert consensus, medication is usually considered when lifestyle changes are insufficient to control symptoms or when PVCs are associated with an increased risk of cardiac events.
For patients with frequent or symptomatic PVCs that are not responsive to medication, catheter ablation may be an option. This procedure involves inserting a catheter into a blood vessel and guiding it to the heart, where radiofrequency energy is used to destroy the tissue causing the PVCs. Catheter ablation has been shown to be highly effective in eliminating PVCs, but it is an invasive procedure with potential risks. Leading experts in electrophysiology suggest that catheter ablation should be considered for patients with drug-refractory PVCs who are experiencing significant symptoms or who are at risk of developing PVC-induced cardiomyopathy.
It’s also important to address any underlying medical conditions that may be contributing to PVCs, such as electrolyte imbalances or thyroid disorders. Correcting these underlying issues can often reduce or eliminate PVCs. Regular follow-up with a cardiologist is essential to monitor PVCs and adjust treatment as needed. Patients should also be educated about their condition and empowered to take an active role in their care.
Navigating the World of PVCs
In conclusion, understanding premature ventricular contractions and their associated ICD-10 codes is crucial for accurate diagnosis, effective management, and appropriate medical billing. This comprehensive guide has provided a detailed overview of PVCs, including their definition, causes, symptoms, diagnostic procedures, treatment options, and ICD-10 coding. By equipping yourself with this knowledge, you can better understand your condition and work with your healthcare provider to develop a personalized treatment plan.
As research continues to advance our understanding of PVCs and their impact on cardiovascular health, it is important to stay informed about the latest developments and treatment options. If you are experiencing frequent or symptomatic PVCs, it is essential to seek medical attention and discuss your concerns with a qualified healthcare professional. Share your experiences with premature ventricular contractions in the comments below, and let’s learn from each other’s journeys toward better heart health.
